Retinal Detachment
A detached retina? Most of us have heard about it happening to someone and realise that it is a serious thing to happen.
But how or why does a retina detach? They are rather firmly stuck onto the back of your eyeball. Aren't they?
The retina is actually a very thin layer of tissue, facing the clear vitreous humour on one side and attached to the choroid layer on the other. Like an onion, the eye is made up of layers that can in unfortunate circumstances, peel apart.
There are three typical causes of retinal detachment:
Retinal holes and tears
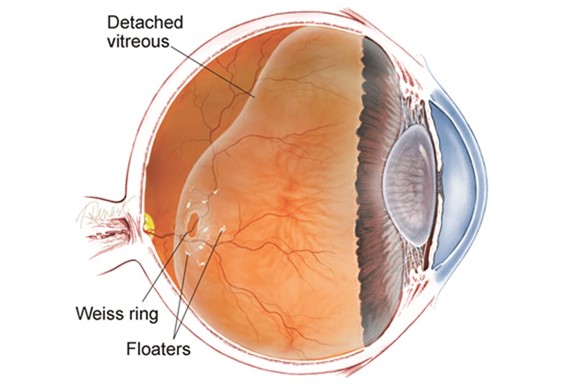
The commonest way a retina can detach is from a retinal tear (retinal break) most commonly caused by a posterior vitreous detachment (PVD). A PVD is when the vitreous humour separates from the retina causing a break or hole in the retinal layer. This gap in the retina allows fluid to leak between the retinal layers, causing the retina to detach.
The symptoms of a PVD and retinal detachment are very similar. Although many people have PVD without developing a retinal detachment, it is always important to have your eye examined if you experience any of the symptoms listed in the next section. A bang or blow to the head cannot cause retinal detachment, but a direct blow to the eye may do.
Holes in the retina are often the result of age-related changes to your eye and are often unavoidable.
Scar tissue
Eye conditions such as diabetic retinopathy can result in scar tissue forming on the surface of the retina and inside your vitreous. This scar tissue can then lead to traction (pulling on the retina), causing a detachment.
Fluid
A rare type of retinal detachment happens when fluid from the blood vessels behind the retina leaks between the retinal layers without there being a hole or tear present. This type of detachment happens because of conditions which cause inflammation or tumours.
How can we help at the Hampshire Eye Clinic?
If you experience any of the symptoms from the list below and would like an honest, friendly and professional opinion, contact us using the form provided, via email info@privateophthalmologist.co.uk or call 07949 767906. These symptoms can happen in other conditions and we can guide you to the most appropriate care.
- Floaters for the first time or more floaters than you had before? The new floaters are usually noticed suddenly. There may be lots of new floaters or commonly a large cobweb-like floater
- Flashes of light in your vision, usually like brief ‘streaks’ of light in your side (peripheral) vision
- Blurred vision
- A dark shadow in your vision
Retinal detachments are rare; only about one in 10,000 people have one each year. Retinal detachment is very rare in children under the age of 16. Increasing age is the biggest risk factor with most retinal detachments happening after the age of 60.
If you are short-sighted, you may be at increased risk of developing a detachment at a younger age. This is because your vitreous gel can become less firm and detach from the back of your eye earlier, causing a tear to form.
You have an increased risk of retinal detachment if you:
- are very short-sighted (more than minus 6.00 D – your optometrist will be able to tell you how short-sighted you are)
- have had trauma (an injury or a blow) directly to your eye
- have already had a detachment in one eye (between two and 10 per cent of people have detachments in both eyes)
- have a family history of retinal detachment.
Treatment for a detached retina
This involves surgery to re-attach the retina to the back of the eye. If caught early, the detachment may not have formed and treatment can take the form of laser. Laser retinopexy can adequately treat a tear before it becomes a detachment. This can be done efficiently and easily at the Hampshire Eye Surgeon. If the retina has unfortunately detached, we can make arrangements and referral for surgery. The sooner surgery is carried out the better the results are likely to be.
Surgery for retinal detachment is complicated and individual to each person’s eye. The type of treatment you may need depends on the type of detachment and factors such as any other eye conditions you may have.
Vitrectomy
The most common surgery used for a retinal detachment in the UK is a vitrectomy. The surgeon reattaches the area of your retina that has become detached, removing some of the vitreous gel in your eye and replacing it with a gas bubble or silicone oil. The gas bubble holds your retina in place against the inside of your eye while it heals.
The gas slowly disappears over about six weeks following the operation. The oil, however, will need a further procedure to remove it at some point in the future.
Scleral buckle
The sclera is the white outer layer of your eye.
A scleral buckle involves attaching a tiny piece of silicone sponge or harder plastic to the outside white of your eye. This presses on the outside of the eye, causing the inside of your eye to slightly move inwards. This pushes the inside of the eye against the detached retina and into a position which helps the retina to reattach. Cryotherapy or laser treatment is then used to seal the area around the detachment. The buckle is usually left in place permanently and can’t be seen once surgery is finished.
Pneumatic retinopexy (gas bubble surgery)
If your retinal detachment is small and uncomplicated, a gas bubble can be injected into the vitreous of the eye, without removing any of the vitreous. This bubble then presses the retina back in place, and cryotherapy or laser is applied round the hole or tear. The gas is reabsorbed over a period of weeks and the retina remains in place. Depending on the size and position of the bubble, your vision may be very blurred in the first few weeks. This type of surgery has been found to be less successful than other types and is not often done in the UK.
FAQs
If you have had a gas bubble put into your eye, your vision will be very blurry for a while, but this is temporary. As the gas is absorbed, you may see a wavy line across your vision, which is the divide between the gas and liquid content of your eye.
Above the line you may be able to see, but below the line your sight will be poor. The line will move, like a spirit level, when you move your head. As the gas disappears, the line across your vision will move downwards, until it becomes a small round dot, which will also disappear with time.
There are different gases that can be used and these are replaced by the fluid in your eye at different rates, some over two to three weeks, and others over about six to eight weeks. While the gas is in your eye and your eye is recovering from the operation, your sight may not be good.
Even if a gas bubble wasn’t used for your operation, your vision may be blurry for a number of days, possibly weeks, following the surgery. During this time you don’t have to limit how much you use your eyes, so watching TV or reading will not cause any problems. It usually takes about six to eight weeks for your eye to recover from surgery and for you and your ophthalmologist to get an idea of the outcome.
Your surgeon will tell you which activities you should avoid after your operation. The advice may be different depending on the type of surgery you have had. Most people will have some restrictions for the first few weeks after the operation.
The length of these restrictions will depend on the procedure you have had, whether you work, and what work you do. For instance, you might find driving difficult while your eye recovers or while you have a gas bubble. Your ophthalmologist can consider all the factors in your case and offer you the best advice about any necessary restrictions.
If you have had gas inserted into your eye, you should not take a flight in an aeroplane while the gas is still in place. The change in pressure in a plane may cause the gas to expand, which would be dangerous for your eye.
Once your eye has healed from the operation, you can continue the sports or activities you enjoy. Full contact sports which may result in a blow to the eye, such as boxing, kick-boxing and martial arts aren’t recommended for someone who has had retinal reattachment surgery.
Posturing is lying or sitting with your head in a certain position. You may be asked to do this before surgery to stop a retinal detachment affecting more of your retina, or after your operation to help keep a gas bubble in place. This is so that the gas bubble continues to put pressure on the part of the retina being reattached. You may need to posture for up to 10 days after your surgery. If you need to do this, your ophthalmologist will explain how to lie or sit and for how long.
You may find it useful to have someone to help you at home while you are posturing. But if that is not possible, and you are worried about coping, let us know, as we may be able to arrange for some help.
Surgery is usually very successful at reattaching the retina, but how well your vision recovers depends on a number of things:
• how much of your retina detached
• if your macula was detached
• if you have another eye condition, such as diabetic retinopathy.
If your macula, which allows you to see fine detail, remained attached, then results are often very good and your central vision may not be affected at all.
If you had a shadow in your peripheral vision, this will disappear after surgery. You may be left with some changes in your peripheral vision, which can be picked up by an eye examination, although you may not notice these on a day-to-day basis.
If your macula detached, but surgery was carried out quickly, then your central vision can return, but it may be distorted. You will probably adapt to this distortion with time, especially if you have good vision in your other eye.
Unfortunately, for some people, surgery may be successful at reattaching the retina, but it may not bring back detailed central vision or areas of peripheral vision. This can happen in any circumstance, but the risk is higher the longer the retina has been detached without any surgery.
If you experience any of the symptoms from the list above and would like an honest, friendly and professional opinion, contact us using the form provided, via email info@privateophthalmologist.co.uk or call 07949 767906. These symptoms can happen in other conditions and we can guide you to the most appropriate care.
Quality care in a relaxing surrounding
Book an appointment to see Mr Nish Srikantha at the Candover clinic in Basingstoke, or the Healthshare Clinic in Winchester.
Both locations are modern purpose built private hospitals designed entirely for patient well-being and comfort. The Candover Clinic is a stand-alone unit located on the Basingstoke and North Hampshire Hospital. The Healthshare Clinic on the outskirts of Winchester boasts a purpose built ophthalmic outpatients department and operating theatre offering the latest diagnostic and treatment technologies.